This study introduces a new method for monitoring and controlling the temperature of the retina during laser treatments, using a technique that measures the electrical responses of pigs’ eyes to light. This approach aims to make retina laser treatments safer and more effective by ensuring the temperature remains at a level that is beneficial without causing damage. The research demonstrates the potential of this focal ERG-based technique both ex vivo and in vivo for improving the heat treatments for retinal diseases, offering a more controlled and personalized approach to patient care.
Kaikkonen, O., Turunen, T. T., Meller, A., Ahlgren, J. & Koskelainen, A. Retinal temperature determination based on photopic porcine electroretinogram. IEEE Trans. Biomed. Eng. PP, (2021). DOI: 10.1109/TBME.2021.3111533
Abstract:
Objective: Subthreshold retinal laser therapy (SLT) is a treatment modality where the temperature of the retinal pigment epithelium (RPE) is briefly elevated to trigger the therapeutic benefits of sublethal heat shock. However, the temperature elevation induced by a laser exposure varies between patients due to individual differences in RPE pigmentation and choroidal perfusion. This study describes an electroretinography (ERG)-based method for controlling the temperature elevation during SLT.
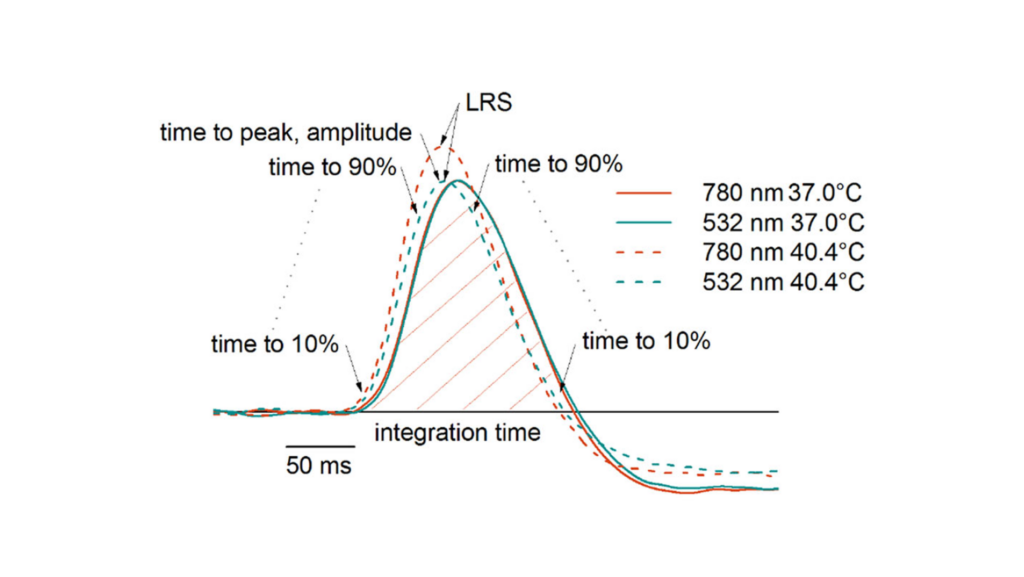
Methods: The temperature dependence of the photopic ERG response kinetics were investigated both ex vivo with isolated pig retinas and in vivo with anesthetized pigs by altering the temperature of the subject and recording ERG in different temperatures. A model was created for ERG-based temperature estimation and the feasibility of the model for controlling SLT was assessed through computational simulations.
Results: The kinetics of the photopic in vivo flash ERG signaling accelerated between 3.6 and 4.7%/°C, depending on the strength of the stimulus. The temperature dependence was 5.0%/°C in the entire investigated range of 33 to 44°C in ex vivo ERG. The simulations showed that the method is suitable for determining the steady-state temperature elevation in SLT treatments with a sufficiently long laser exposure and large spot size, e.g., during > 30 s laser exposures with > 3 mm stimulus spot diameter.
Conclusions: The described ERG-based temperature estimation model could be used to control SLT treatments such as transpupillary thermotherapy. Significance: The introduced ERG-based method for controlling SLT could improve the repeatability, safety, and efficacy of the treatment of various retinal disorders.